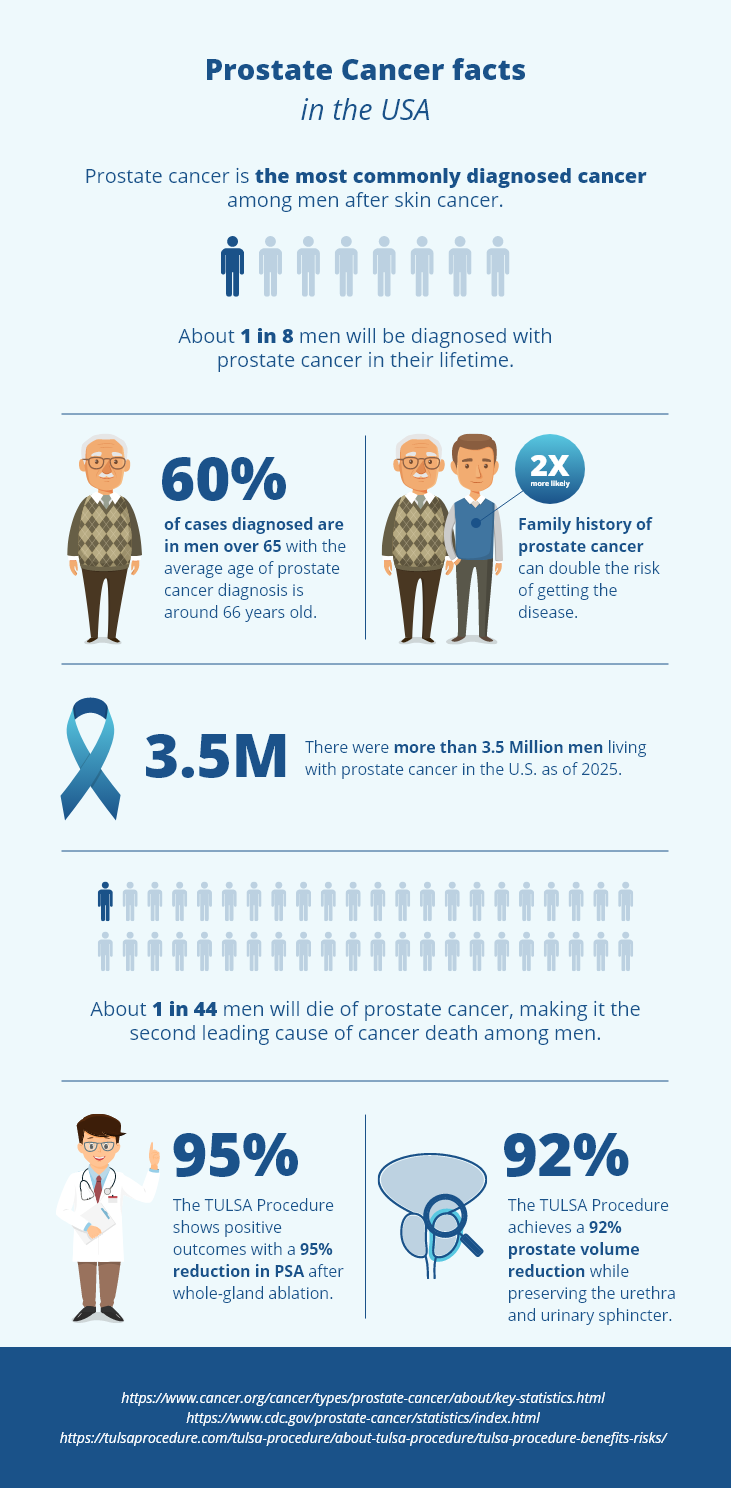
Prostate cancer is the second most common form of cancer in men in the U.S., after skin cancer. It’s also the second leading cause of cancer-related death in men.
- The American Cancer Society estimates about 313,780 new cases of prostate cancer in 2025.
- It also projects approximately 35,770 deaths from prostate cancer in the same year.
- This translates to about 1 in 8 men being diagnosed with prostate cancer during their lifetime. But each man’s risk of prostate cancer can vary, based on his age, race/ethnicity, and other factors. For example, black men face a higher risk, with estimates showing about 1 in 6 will be diagnosed during their lifetime.
At Profound Medical, we’re committed to supporting men’s health and encouraging early action during Prostate Cancer Awareness Month. Our goal is to educate the public about the importance of early screening, especially since prostate cancer often has no symptoms until it reaches a more advanced stage. As well as risk factors, screening options, and the importance of proactive care when it comes to prostate health.
About Prostate Cancer
The prostate is a small gland, about the size of a walnut, located just below the bladder. It surrounds the urethra, the tube that carries urine out of the body, and plays a vital role in producing the fluid that makes up semen.
Prostate cancer develops when cells in the prostate begin to grow uncontrollably. In some cases, it grows slowly and may not cause issues right away. In others, it can be more aggressive and spread to nearby tissues, bones, or other organs.
Raising prostate cancer awareness helps more men understand how the prostate works, what changes to look out for, and when to talk to a doctor. Early understanding and regular screening are key parts of protecting your long-term health.
Who’s at Risk?
Several factors can raise your risk for prostate cancer:
- Family history – If your father or brother has had prostate cancer, your risk is higher.
- Age – The average age of diagnosis is 66. It’s rare in men under 40.
- Race – The American Cancer Society cites that African-American men have a higher risk and are more likely to be diagnosed at an advanced stage.
Why Awareness Month Matters
Prostate Cancer Awareness Month is observed every September. It’s an opportunity for patients, families, doctors, and advocates to come together and shed light on this important health issue. Here’s why it matters:
- Education – It helps men understand the risks, symptoms, and importance of regular checkups.
- Early detection – Catching prostate cancer early—before it spreads—can give patients more options and better outcomes.
- Informed choices – Patients can learn about a range of treatment options for prostate disease, including less invasive approaches.
- Support – Stories shared by survivors and families offer hope and encouragement to others.
- Research – Increased awareness brings more attention and funding for studies that may lead to improved future treatments.
- Healthy habits – It’s a great time to focus on lifestyle choices, such as diet and exercise, that can benefit overall prostate health.
How to Observe Prostate Cancer Awareness Month
During the month of September, local and national organizations take part in activities to raise awareness of prostate cancer. Here’s what you can do to participate and help spread awareness about prostate cancer:
- Talk to your partner, family member, or friend about prostate health.
- Share posts, blogs, and resources on social media dedicated to raising awareness about prostate cancer.
- Visit Men’s Health Network to read about facts and statistics.
- Stay updated with the American Cancer Society on the latest statistics.
- If you’re a male aged 40 years or older, talk to your doctor about your risk factors for prostate cancer.
- Take a proactive step by completing an IPSS Symptom Quiz and sharing the results with your doctor.
Stay Informed. Stay Proactive This September
Understanding the risks and recognizing early signs are key steps in protecting prostate health. Supporting prostate cancer awareness means starting conversations, encouraging regular screenings, and staying informed about available care options.
For those exploring treatment paths for prostate disease, the TULSA Procedure may be an option worth discussing with a physician. It’s a minimally invasive approach that uses the TULSA-PRO® system to ablate a surgeon-defined region of the prostate, with the goal of preserving urinary and sexual function.
This September, stay informed and proactive by learning more or starting the conversation with your family or physician.
Frequently Asked Questions
What is the Gleason Score, and why does it matter?
The Gleason Score is a tool doctors use to better understand how aggressive prostate cancer may be. It’s determined by looking at prostate tissue under a microscope and grading the two most common patterns of cancer cells on a scale from 1 to 5. These two numbers are added together to get a score between 6 and 10.
- Lower scores (such as 6) suggest a slow-growing cancer.
- Higher scores (such as 8 to 10) indicate faster-growing, more aggressive cancer.
The Gleason Score plays a key role in helping doctors decide what treatment plan may be best for each individual patient.
Can BPH turn into prostate Cancer?
BPH, or benign prostatic hyperplasia, is not cancer and does not develop into prostate cancer. However, both conditions can exist at the same time.
That’s why routine prostate screenings, like the PSA test and digital rectal exam, are important. They help detect changes early, even when symptoms may be similar or not present at all.
Why is early detection of prostate cancer so important?
In many cases, prostate cancer doesn’t cause noticeable symptoms in its early stages. Without screening, it can go undetected until it becomes more advanced and harder to treat.
Early detection gives patients more options and may lead to better outcomes. If you’re at increased risk due to age, family history, or race, talk to your doctor about when to start screening.
What is the TULSA Procedure?
The TULSA Procedure stands for Transurethral Ultrasound Ablation. It’s a minimally invasive approach used to ablate (remove) a surgeon-defined region of the prostate using precise, directional ultrasound energy.
The procedure is:
- Radiation-free and incision-free
- Performed in an MRI suite with real-time imaging
- FDA-cleared and customizable based on clinical needs
It utilizes the TULSA-PRO system to deliver controlled heat to targeted areas of the prostate, while protecting nearby structures, such as the urethra and rectum. The goal is to treat diseased tissue while helping preserve urinary and sexual function.
Jul 31, 2025 | Cole Parrish
 Find a Center
Find a Center Contact Us
Contact Us