
If so, it is important to have access to comprehensive, in-depth information about your disease and all the treatment options available. In this section, we will give you an overview of what you or a family member should know, to help you feel well-prepared for when you speak with your doctor. Knowing your options may help you approach decisions with peace of mind.
Many men that have prostate cancer have no symptoms. Therefore, prostate cancer typically develops unnoticed in the early stages; there are usually no complaints from the patient. Signs and symptoms only occur at later stages.
Doctors use various diagnostic procedures to determine whether a patient has prostate cancer. The most common tests are listed below.
The multiple diagnostic procedures aim to find out how aggressive the cancer is, how large it is, whether it has spread into the surrounding tissue, and to assess the patient’s overall condition. Various examinations may need to be carried out several times to get the most detailed picture possible.
Prostate Specific Antigen (PSA) is a protein made by prostate tissue. The amount of PSA measured in your blood normally increases with age and prostate size, but abnormally high levels may indicate the need for additional testing1.
The Digital Rectal Exam (DRE) test is performed by the Urologist who will use their gloved index finger to feel your prostate through the rectal wall to assess the size, shape and stiffness of your prostate1.
The Magnetic Resonance Imaging device will use magnets to generate an image of your prostate and surroundings. From this image, the doctor may be able to find regions suspicious for cancer1.
Under imaging guidance (typically ultrasound), a small needle is used to collect a small amount of tissue from the prostate for further examination1.
Prostate cancer is described as a change in the tissue. The prognosis depends on how far the cancer has spread at the time of diagnosis. It can be characterized by ‘more’ or ‘less’ aggressive growth. Doctors use a method of classification called ‘staging’ to summarize the local extent and evidence of the spread of cancer.
The majority of prostate cancers are diagnosed at an early stage, where the cancer is limited to the prostate, meaning it is growing locally within the prostate. Therefore, it’s referred to as localized cancer. In later stages, it can extend outside the prostate, which is referred to as locally advanced cancer, or even metastasize to other organs. It can spread beyond the prostate by:
To recommend an appropriate treatment, doctors assign a stage to each patient’s prostate cancer. Staging is based on the extent of the cancer, whether lymph nodes are affected, and whether the cancer has already spread to other organs².
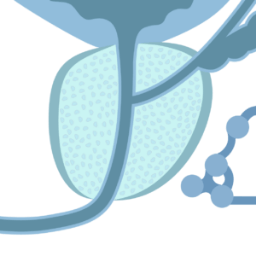
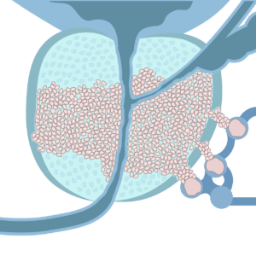
A healthy prostate.
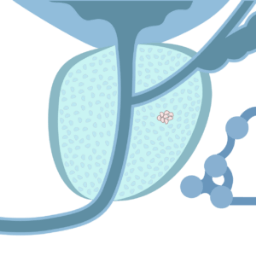
The cancer cannot be felt in a digital rectal examination, and cannot be seen using imaging techniques2.
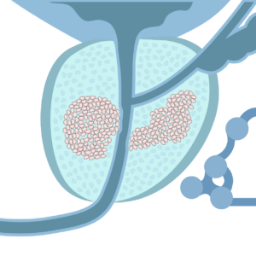
The cancer is limited to the prostate — localized prostate cancer2.
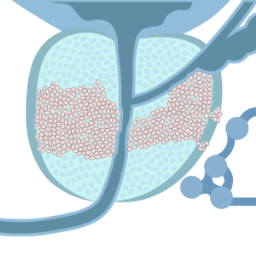
The cancer has broken through the capsule — locally advanced prostate cancer2.
The cancer is growing in surrounding organs2.
Choosing the right treatment for you is not always an easy decision.
Understanding the values and risks associated with available options is essential to helping you make the best decision possible.
The following are some of the most commonly used treatments.
For more information, always speak to your doctor about your diagnosis and what is best for your health and lifestyle.
Many men with prostate cancer do not need to be treated right away because their cancer is slow-growing, and there is a low risk of spreading².
Instead, these men are offered active surveillance, which involves close monitoring of their cancer with repeat PSA, DRE and biopsy tests. Treatment is recommended when there are signs that the cancer has progressed4.
The TULSA Procedure is a less invasive option. It is a customizable, predictable, incision-free and radiation-free ablation of a surgeon defined region of the prostate. It is performed in combination with real-time MR Imaging, transurethral thermal ultrasound and a closed-loop temperature feedback control.
Radical prostatectomy is a surgical procedure (performed robotically or not) that removes the entire prostate gland. If the cancer has spread to surrounding lymph nodes, they too are removed.
Common side effects faced by patients after undergoing prostatectomy include erectile dysfunction and urinary incontinence4.
External beam radiation therapy (EBRT) uses high-energy x-ray beams from outside of the body to ablate cancer cells. Brachytherapy (internal radiation therapy) involves placing radioactive material inside or beside the cancer to ablate cancer cells⁵. Although both healthy and cancerous cells are damaged by radiation therapy, the goal is to destroy as few healthy cells as possible.
Common side effects faced by patients after undergoing radiation therapy include erectile dysfunction and gastrointestinal toxicity4.
1. National Cancer Institute. (2011, August). Understanding Prostate Changes. Retrieved: https://www.cancer.gov/types/prostate/understanding-prostate-changes/prostate-booklet.pdf
2. American Cancer Society. (2015, March 12). Prostate Cancer. Atlanta, GA: American Cancer Society. Retrieved: https://www.cancer.org/acs/groups/cid/documents/webcontent/003134-pdf.pdf.
3. Rukstalis, D. B. (2002). Treatment options after failure of radiation therapy—a review. Reviews in urology, 4(Suppl 2), S12. Retrieved: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1477547/
4. National Cancer Institute. (2019, June 12). Prostate Cancer Treatment. National Cancer Institute. Retrieved: https://www.cancer.gov/types/prostate/patient/prostate-treatment-pdq
5. Radiologyinfo.org (2019, May 01). Brachytherapy. RadiologyInfo.org for Patients.
Retrieved: https://www.radiologyinfo.org/en/info.cfm?pg=brachy