
The Transurethral Ultrasound Ablation (TULSA) Procedure is a minimally invasive procedure that uses directional ultrasound to ablate (destroy) prostate tissue. The procedure is performed in a Magnetic Resonance Imaging (MRI) suite and uses the TULSA-PRO® system to ablate prostate tissue from the ‘inside-out’ (from inside the urethra heating outwards to the edge of the prostate). The procedure is shown to be a well-tolerated, safe option for localized prostate cancer, as shown in a multinational phase 1 study of 30 patients and a subsequent Pivotal study of 115 patients.
Getting Started
At Profound Medical, we refer patients to a TULSO-PRO physician to determine eligibility. For your consultation, you’ll need to provide information regarding your diagnosis, which can include:
- PSA score
- Biopsy report
- Digital rectal exam (DRE)
- MRI information
Once your TULSA-PRO physician has reviewed your medical history and determined that you are a good candidate for the procedure, you’ll meet with them to discuss the next steps. They will explain the benefits and risks of the procedure and work with you to customize a treatment plan.
The Day of the Procedure
The TULSA Procedure happens in 4 stages:
- Preparation – Before the procedure, you will meet the treatment team, including a treating physician and a Radiology Technologist. Your team will make sure you are comfortable before sedation.
- Planning – Your treating physician will use high-precision MR imaging to draw the boundary lines around the areas of your prostate that will be ablated. Boundary lines are drawn out to avoid critical structures around the prostate. This step is tailored to your prostate size, shape, and disease.
- Delivery – The TULSA-PRO system automatically carries out the ablation instructions outlined by the physician, ablating only within the prescribed boundary lines. This helps ensure precise prostate ablation and minimizes the risk of human error.
- Confirmation – Using MR imaging, your treating physician will confirm that the intended areas of the prostate have been successfully ablated. After the procedure, you will be monitored briefly and patients can typically leave the same day.
How the TULSA Procedure Works
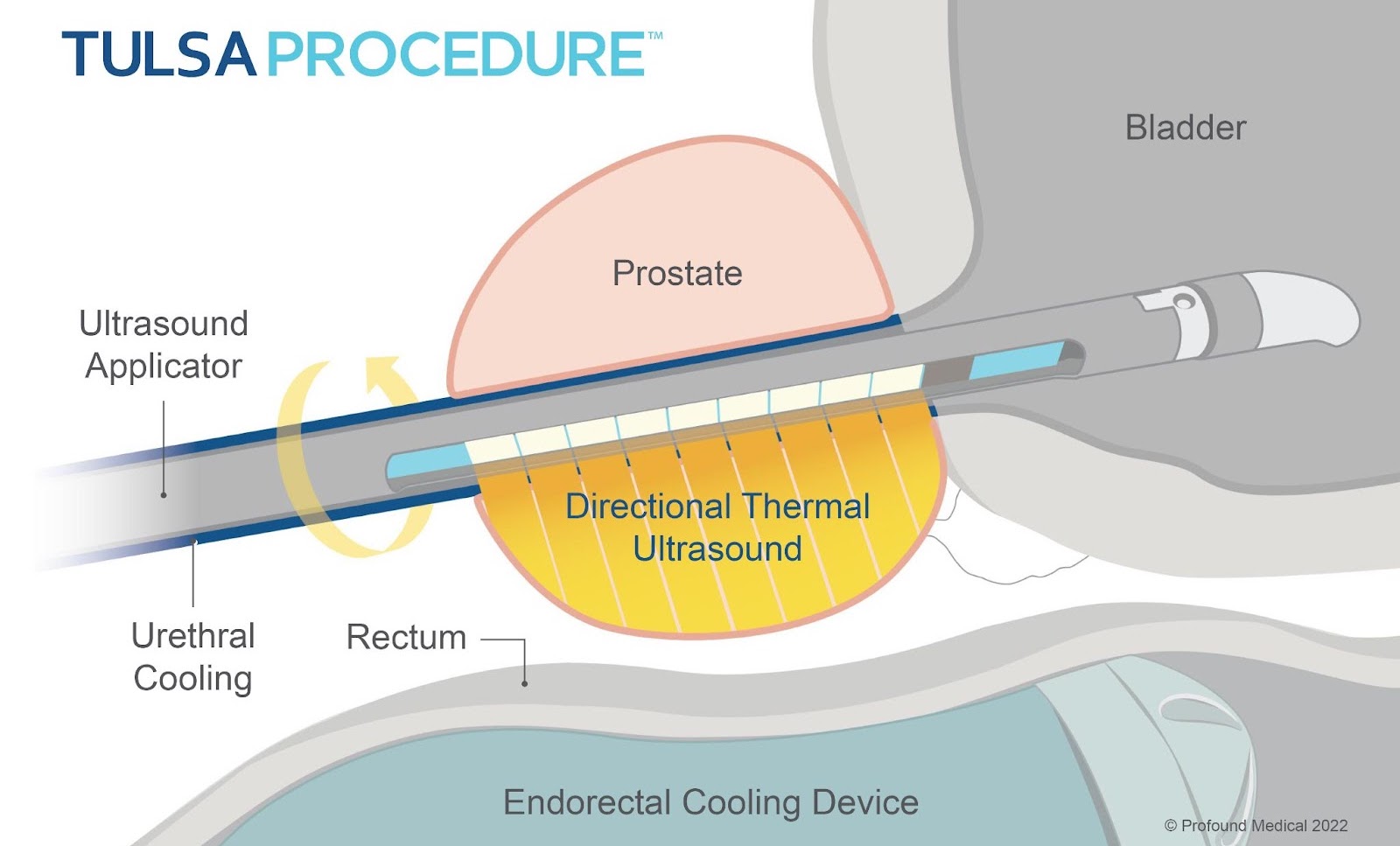
During the delivery stage, the ultrasound applicator (UA) is inserted into the urethra and delivers the ultrasound energy towards the prostate. As the device rotates, it creates a sweeping pattern, traveling outwards towards the edge of the targeted prostate area, and ablates the prostate tissue. This process is referred to as an ‘inside-out’ approach because the directional ultrasound energy comes from the urethra located inside the prostate.
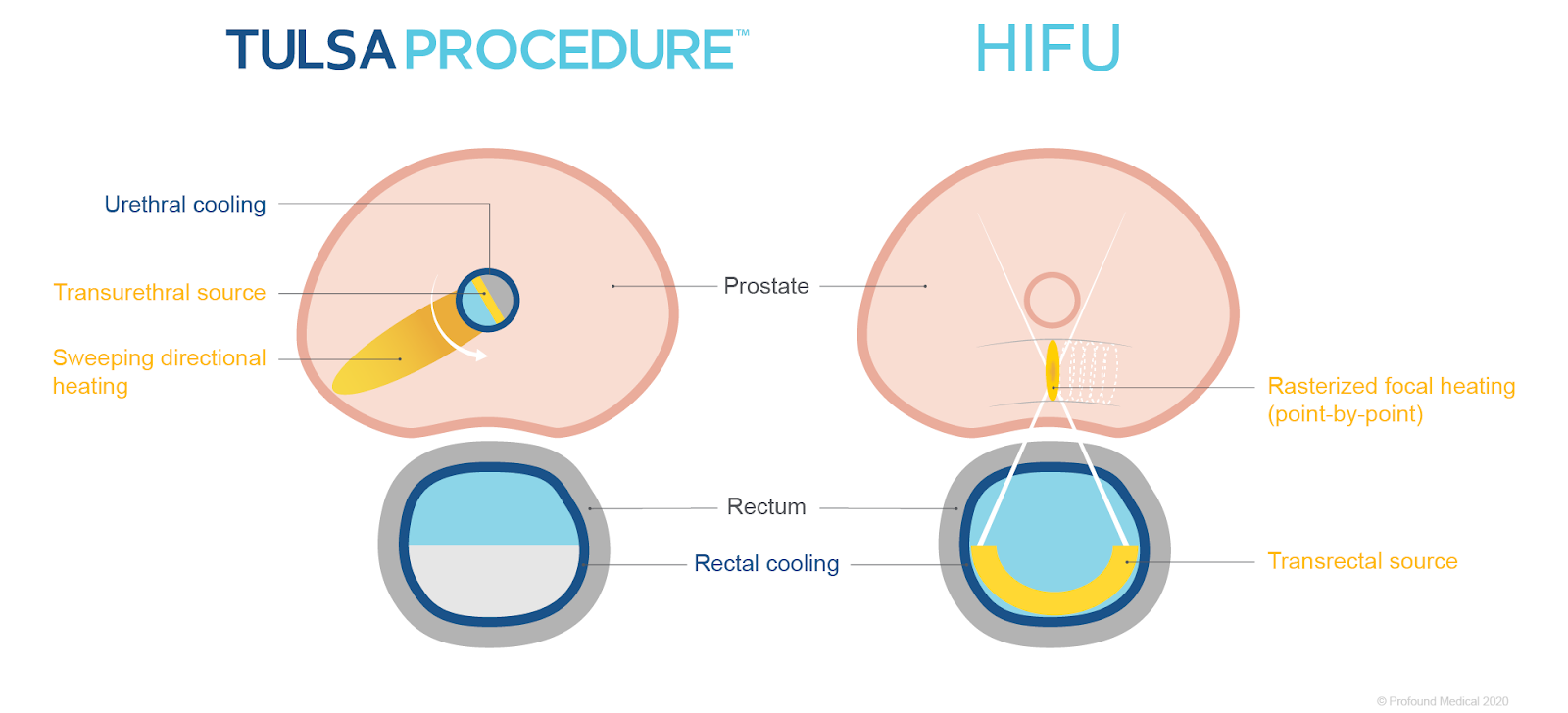
‘Outside-in’ ablation is used in other therapies, such as High-Intensity Focused Ultrasound (HIFU). This approach involves inserting a device containing the energy source inside the rectum, which is located outside of the prostate. The thermal ultrasound energy travels through the rectal wall and the heating pattern created is focused on a particular prostate area. This is referred to as rasterized focal heating or sonication.
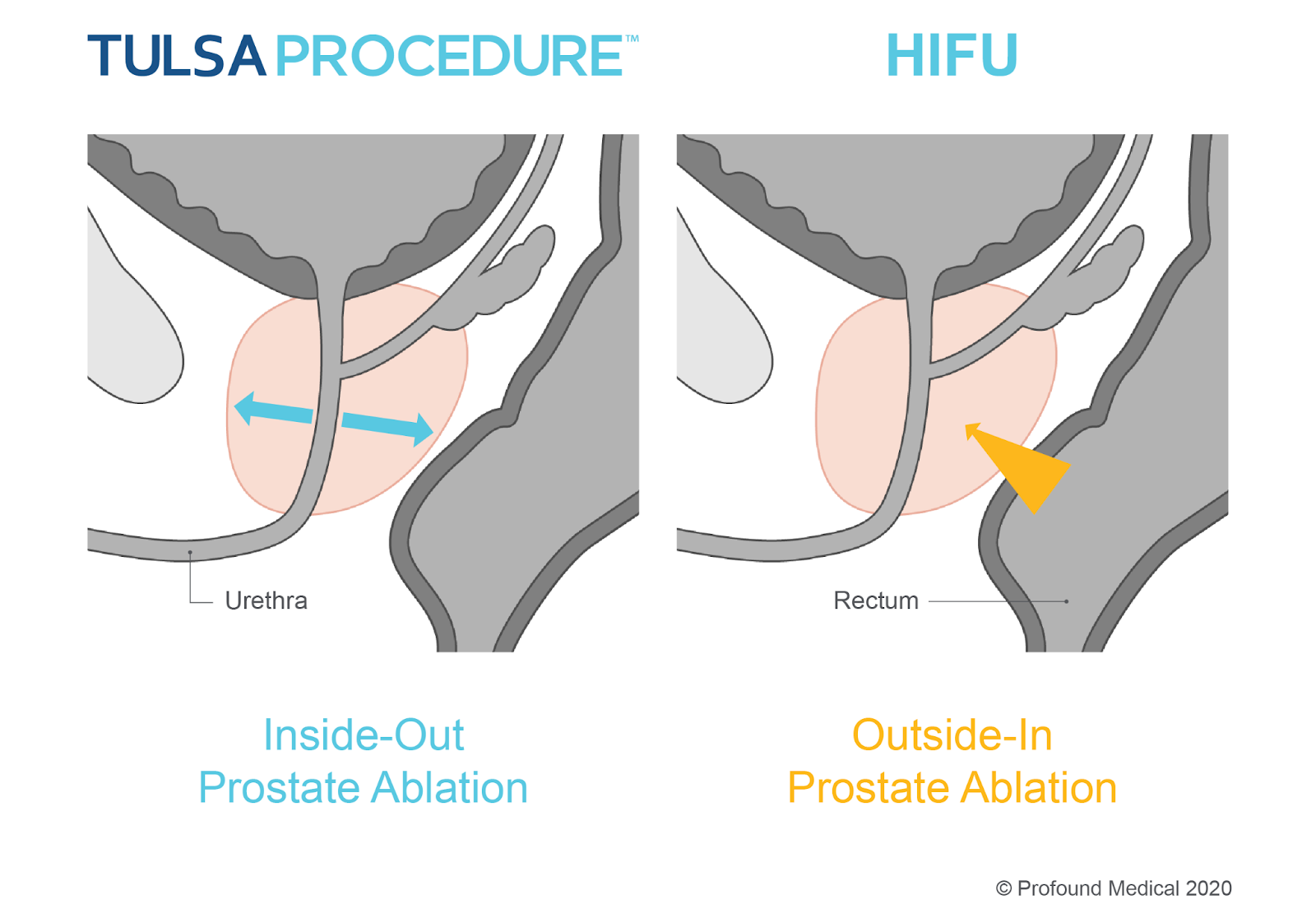
The ability to ablate from the inside-out avoids direct contact with important neurovascular bundles (NVBs), minimizing damage to surrounding tissues and structures, and helping to preserve men’s functional abilities. Your physician can see in real-time what is happening as the procedure takes place within an MRI suite, resulting in a very controlled and predictable environment. The TULSA Procedure also actively cools the urethra and rectum protecting the tissue from the ultrasound energy.
Continued Prostate Care
If you are in need of additional prostate care, you may either have a repeat TULSA Procedure, or choose any other type of prostate therapy to address your prostate needs. The TULSA Procedure does not “burn bridges” as it allows other therapies to be performed after.
References:
- Chin, Joseph L., et al. “Magnetic resonance imaging–guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: a prospective phase 1 clinical trial.” European urology3 (2016): 447-455.
- Klotz, Laurence et al. “Magnetic Resonance Imaging-Guided Transurethral Ultrasound Ablation of Prostate Cancer.” The Journal of urology, 101097JU0000000000001362. 6 Oct. 2020, doi:10.1097/JU.0000000000001362
Nov 15, 2021 | Cole Parrish
 Find a Center
Find a Center Contact Us
Contact Us